If you’ve ever hobbled through intense heel pain, you know how rough and tumble it can get. When you wake up every morning, it strikes the bottom of your foot as you take those first few steps out of bed. It can feel like a nail driving into your foot with each step, and that same pain greets you morning after morning.
Once you put on your shoes with supportive insoles, there’s a bit of relief. But the pain still screams at you throughout the day, whether you’re standing or walking (and with that kind of pain, you can’t even THINK about running or playing sports).
This excruciating pain is none other than the dreaded plantar fasciitis. And in order to better understand its origins and rehabilitation, there’s lots of information to walk through (no pun intended).
What is Plantar Fasciitis?
Let’s start with the basics:
Plantar fasciitis is an injury in a thick band of tissue (called the plantar fascia) that connects your heel bone to your toes. It’s most commonly associated with a stabbing heel pain after waking up (the pain often decreases throughout the day). Over 2 million Americans suffer from plantar fasciitis within a given year, with approximately a 10% occurrence throughout one’s lifetime.
Interestingly enough though, while the suffix “-itis” indicates inflammation, multiple studies have found that there’s actually no cellular evidence of an inflammatory response. Instead, research indicates that the pathology is more properly termed a fasciosis, which is actually a degeneration of tissue — and this degeneration is one of the telling signs that helps to diagnose the injury in the first place.
Of course, since tissue degeneration isn’t visible from the outside, that isn’t the first thing that may cause someone to suspect that they have this particular injury. Instead, there are a few common symptoms that serve as telltale signs.
Common Symptoms of Plantar Fasciitis
Plantar fasciitis isn’t limited solely to that frustrating heel pain in the morning (though it’s incredibly common). Because the plantar fascia runs along the bottom of your foot, there are a number of other symptoms produced by the condition:
- Heel pain after prolonged sitting/laying/non-weight bearing activity
- Tenderness in the medial anterior (middle front) area of the heel bone (protruding outwards)
- Increased pain with longer duration standing/weight bearing activity, walking, running, and going up or down stairs
- Increased pain in the absence of external support from shoes; increased pain when walking barefoot (especially on harder surfaces)
However, although the pain of plantar fasciitis can be both chronic and excruciating, people don’t often seek treatment for it right away. On average, most cases reported experiencing symptoms for 13.3-14.1 months before seeking formal treatment. So, most people deal with this kind of pain for more than a year before the symptoms are bad enough to impede their daily activities. And, naturally, the injury is prone to worsening the longer it’s left untreated.
But that’s skipping ahead — let’s get down to the anatomy to more thoroughly understand what’s actually being affected (and why).
Anatomical Breakdown
As mentioned before, the plantar fascia is considered to be the tissue that runs along the bottom of your foot. But in all actuality, this particular tissue isn’t technically a fascia.
A fascia is a kind of tissue that surrounds your muscles that helps with absorbing forces. Basically, during physical activity, it absorbs the external forces that impact your body and displaces them throughout the entire muscle.
However, in the case of the plantar fascia, using the term fascia is actually a misnomer. It’s much closer to a tendinous aponeurosis: a type of thin connective tissue that helps connect muscles to bone. Unlike fascia, an aponeurosis shares mechanical and histological properties with ligaments and tendons. (That being said, aponeuroses are still thin tissues that can surround muscles or organs like fascia, so it’s an understandable misconception.)
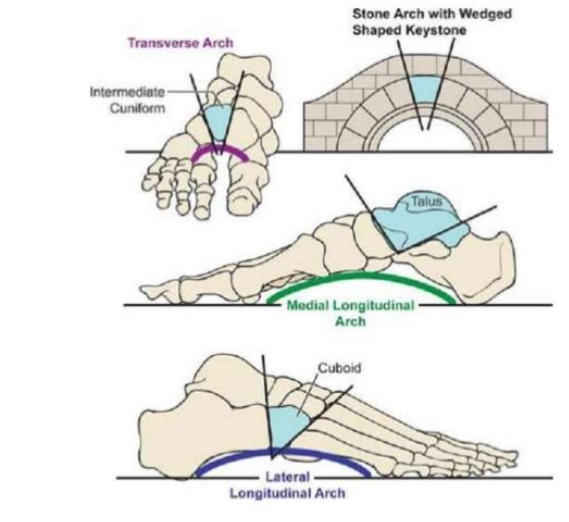
Studies show that the plantar fascia/aponeurosis supports both the medial longitudinal arch and the transverse arch, as is shown in the image to the right. By supporting the medial longitudinal arch, it supports the midfoot and prevents it from collapsing into excessive pronation. And its support of the transverse arch helps to prevent your metatarsals (toe bones) from splaying excessively.
The pull of the plantar fascia increases the compressive forces placed on the arch, which is what allows it to support the foot in the first place. When greater tension is placed upon the plantar fascia (like during higher level activities), the fascia will modify the stiffness of the arch to match the load of the activity — meaning that it will adjust your foot’s structural stability in response to higher loads.

Some studies have shown that the plantar fascia can withstand very high loading without tearing. On average, the ultimate strength of the fascia was found to be 1189 ± 244N, which basically means the tissue could bear the average weight of about 276 pounds before breaking.
Pretty impressive, right? Something as small and thin as the plantar fascia is not only capable of providing foot stability and withstanding high levels of force, but it can also respond to changing weight-bearing activity.
But then that begs the question: if the plantar fascia is so strong, how does it manage to get so damaged, and for so long?
Causes of Plantar Fasciitis
Despite the tissue being impressively strong, plantar fasciitis is still theorized to occur as a result of mechanical overload. Just because the tissue can handle high loads without tearing doesn’t mean it can handle it often. The fascia typically begins to degenerate when it undergoes prolonged overloading and struggles to keep up with the demand of external stressors.
This kind of overloading places excessive strain on the fascia, creating microtears in the tissue (which is that degeneration mentioned earlier). Consequently, the tissue is unable to repair itself, and the repeated attempts of healing creates fibrosis, or a scarring of the tissue.
In many cases of plantar fasciitis, individuals shared one major commonality: the plantar fascia itself had increased in thickness. This thickening of the fascia occurs when people experience a significant degree of build-up in the tissue due to fibrosis. Unfortunately, since most people don’t seek medical treatment until more than a year of experiencing symptoms or pain, this build-up is quite common.
Later studies found that the thickness of the plantar fascia was directly correlated with changes in pain, meaning that, as the thickness increased, the pain would as well. (But it works the other way, too — as the plantar fascia decreases in thickness, the degeneration of tissue will slow down, thus allowing the tissue to start repairing itself again.)
However, while frequent overloading is the primary culprit for causing plantar fasciitis, it doesn’t work alone — we can’t forget about those pesky risk factors, now can we?
Common Risk Factors
As previously referenced, plantar fasciitis affects quite a large segment of the population — but some people are certainly more prone to experiencing it relative to others.
For example, about 22% of athletes endure plantar fasciitis pain as a result of participating in activities that involve higher forces and an increase in workload.
More specifically, athletes involved in sports like running, soccer, gymnastics, and dance are known to be at higher risk. Both runners and soccer players are prone to this foot injury as a result of higher mileage, whereas gymnasts and dancers typically endure the injury as a result of their footwear not providing enough support for their feet.
In the working, non-athlete population, plantar fasciitis is often found in individuals whose jobs involve walking or standing on hard surfaces for extended periods of time, or for those who frequently jump in and out of vehicles (such as delivery trucks or construction machinery).
And that’s just some common populations who are prone to the injury; there are also a number of physical attributes that can put you more at risk of developing or worsening plantar fasciitis, too.
For example, people who have higher body mass index may be more at risk because their feet have to absorb higher forces on a daily basis, thus building up strain on the plantar fascia over time. Or, people who have a leg-length discrepancy may experience plantar fascia in the longer leg, as this foot will undergo an increased load compared to the shorter leg.
Of course, there are also some foot-specific physical characteristics that can contribute to the injury.
Often, people who have plantar fasciitis have a limited range of motion for dorsiflexion (when you lift the foot up towards your shin). This typically occurs when there is hypomobility at your ankle joint, meaning that your ligaments are either too short or too tight to allow your foot to move at its full capacity. As a result, your foot will try to increase its range of motion by pronating the foot (collapsing the medial arch), which ends up adding excess strain on the already-tight plantar fascia and puts it at risk of overloading.
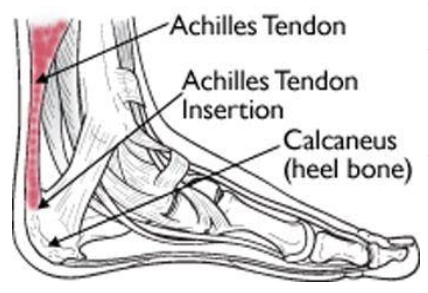
Additionally, a lack of flexibility in certain leg muscles can also potentially factor into risk of plantar fasciitis. The primary muscles for plantar flexion (when you point your toes down and away from your shin) connect to the Achilles tendon, which is connected to the calcaneus (heel bone). Remember: the plantar fascia is also attached to the calcaneus, so if your plantar flexors lack adequate length, they may pull on the Achilles tendon, which in turn also pulls the calcaneus, ultimately placing strain on the plantar fascia.
Some people are also at risk of plantar fasciitis if they have certain foot deformities, like “pes cavus” or “pes planus.” Pes cavus is when the main arch of your foot is much higher than usual; this heightened arch prevents your foot from pronating naturally, thus affecting shock absorption and causing excess strain on the fascia. Pes planus, however, has a decreased arch height that doesn’t allow for proper arch strength or stability.
Whew! That was a lot of risk factors — but they all have one thing in common. Developing plantar fasciitis is heavily dependent on the amount of strain and tension on the tissue.
But enough about the dangers! Let’s talk prognosis and treatment; you’re deserving of some positive (and thoroughly informational) news.
Prognosis and Treatment of Plantar Fasciitis
Although it often takes people a while to seek treatment for plantar fasciitis, it’s still an entirely treatable injury! The rehabilitation process may take a bit of time, but it still has a high rate of recovery — approximately 90% of plantar fasciitis cases were able to alleviate their symptoms with conservative care (i.e., physical therapy, ultrasound, orthoses, etc.). Only about 10% of cases end up having to resort to surgical intervention to resolve their pain, and generally, surgery on the plantar fascia is only recommended if conservative care has proven ineffective.
Additionally, about 80% of reported cases have entirely resolved their symptoms within just 12 months following outpatient clinical courses. And, with a proper therapy program and functional training sessions, people can typically lessen their symptoms much quicker!
If you’re curious to know more about what a “proper” therapy program looks like, look no further — we’ve got the perfect, in-depth breakdown for you.
Treatment from a Medical Professional
In a comprehensive rehabilitation program, your physical therapist will hone your treatment plan to address any risk factors or deficits in your foot’s functionality. This means tackling a number of different facets of movement, including range of motion, structural stability, and shock absorption.

As mentioned before, limited dorsiflexion is a huge contributor to the overloading of your plantar fascia, so dorsiflexion mobilization is key for treatment! Both the ankle joint and the soft tissue surrounding it require attention; typically, performing a trigger point massage in the soft tissue of your calves and plantar flexors can lead to improvements in overall foot function. And, in tandem with daily stretching exercises, these massages are known to lessen patients’ overall pain.
Along with mobilization and stretching, your treatment should also include an ample strength training program to improve the foot core (which will ultimately reduce the overloading on the plantar fascia). The foot core consists of multiple muscles: the intrinsic foot muscles, the calf complex, and the posterior tibialis muscle. Each of these muscles help to absorb forces, to stabilize the arch of the foot, and to produce functional movements.
Muscles like the posterior tibialis play an important role in sharing the load of forces and providing extra stability for the arch, thus reducing the strain on the plantar fascia. So, strengthening these supportive muscles are imperative for maintaining foot stability and relieving the fascia from bearing the load by itself.
Sport-Specific Screening for Athletes
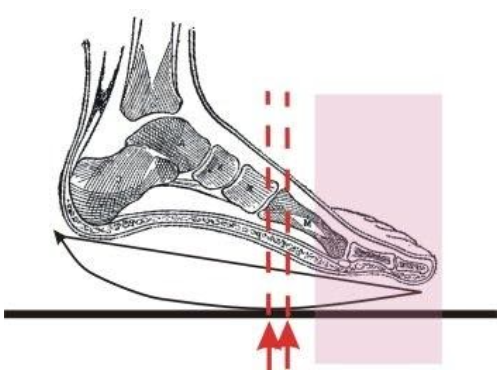
This extra support isn’t just necessary when the foot is in neutral position — it’s just as important while you’re walking or running (arguably moreso). In particular, the terminal stance of your walking or running gait (when the heel begins to lift off of the ground) typically places a lot of demand on the plantar fascia if the arch of your foot lacks support.
In addition to strengthening, it’s also key to assess your lower extremity alignment in order to improve shock absorption. If larger leg muscles (like calves, quadriceps, or hip muscles) aren’t providing ample shock loading and alignment, your body will try to displace the pressure of external forces — and that typically means the plantar fascia.
For runners and other athletes in particular, it is useful to go through a full biomechanical movement evaluation. By testing your movement through sport-specific activities, your physical therapist will have a more thorough understanding of what movement patterns need to be improved upon in order to reduce plantar fascia stress.
Ultimately, this knowledge can have a major impact on your overall performance — if you think about it, each mile you run can be anywhere from 1,000 to 2,000 steps, so if you improve the mechanics of each step landing, that’ll provide a HUGE reduction of stress on your plantar fascia for every mile you run!
And there you have it — a comprehensive treatment plan to finally put an end to that frustrating plantar fasciitis pain. When seeking treatment for a pain as persistent as plantar fasciitis, it’s the most beneficial to work with a specialist who addresses ALL of these aspects of movement, that way your feet and ankles are rehabilitating as a whole.
Fact-Checking Common Plantar Fasciitis Treatments
With all of this in mind, though, don’t think that physical therapy is the only type of treatment that can alleviate your pain! (After all, that’d be super frustrating if you didn’t have the time or access to a solid physical therapy clinic.)
As mentioned before, plantar fasciitis is an injury that is frequently left untreated for quite some time. Naturally, throughout the time prior to seeking treatment, people will resort to a number of home remedies and alternative treatments to cope with the pain.
Let’s review some common alternate methods to see whether or not they can actually help with pain relief and healing for plantar fasciitis.
Temporary Orthotics
Using orthotics can actually be pretty beneficial for plantar fasciitis (some physical therapists will even use them during rehab). Orthotics for the foot are almost akin to training wheels for a bike — they provide temporary stability for the arch and plantar fascia, which can help reduce your overall pain and overloading on the fascia. This extra stability boost also gives your surrounding foot structures a chance for improving their own mobility and stability as well.

You can purchase either custom or store-bought orthotics; both are proven to yield similar results in temporarily lessening overall pain. Plus, they’ve been shown to improve walking mechanics in the short-term!
Another bonus is how easily you can access orthotics. Most local sport stores will carry orthotics — for plantar fasciitis specifically, it’s best to get medial arch supportive insoles. That being said, your foot still has to pronate to properly absorb forces, so make sure the insoles you purchase aren’t too rigid! (Otherwise you’re essentially just heightening your arch without any force reduction, and that’s all bad.)
Taping
Similar to orthotics, taping your feet can be a helpful temporary remedy. Because it can help with reducing the pain and overall stress placed on the plantar fascia, taping can temporarily improve an individual’s functionality. In fact, if it’s necessary, taping for plantar heel pain can be effective for up to three weeks.
Some physical therapists will encourage taping during the rehabilitation process, particularly when introducing you to a new strength program. As long as the injury isn’t too painful, the extra support from the taping will allow your foot to focus less on stability and more on improving its strength deficits.
Of course, taping is very much a temporary solution — while it can assist in expediting the therapy process, it’s primarily only effective for short-term pain relief. (Besides, even if it was more long-term, no one wants to have to tape their feet for the rest of their life.)
Night Splints
Lo and behold — another great short-term method for pain relief!
Night splints are a type of foot brace that holds your foot in a steady position with your toes pointing upwards. This position is meant to apply a consistent, gentle stretch for your plantar fascia. It also stretches out your Achilles tendon to prevent it from contracting (and pulling on the calcaneus, as mentioned before).

You can wear night splints every night while you sleep for anywhere between 1 to 3 months. They typically improve heel and plantar fasciitis pain throughout the time you wear them. It’s especially helpful for those who experience pain in the first few steps when they get up in the morning.
Cortisone Shots
This is one remedy that’s a bit too dicey to recommend.
Cortisone is primarily used to reduce inflammation — and, as mentioned before, plantar fasciitis is a degenerative process involving tears in the tissue, rather than inflammation. There’s very limited evidence that proves whether or not cortisone shots help with plantar fasciitis pain or healing.
In fact, several studies have reported that cortisone can impose new risks on the plantar fascia. Following multiple cortisone shots, the plantar fascia can actually be prone to rupture (yikes). This is theorized to be a result of cortisone’s ability to stop inflammation, as it often shuts down healing or regenerative processes in order to do so.
So the next time you’re dealing with plantar fasciitis, consider keeping the cortisone on the shelf — there are better, less risky methods to cope with that heel pain.
Self-Massage
Here’s a remedy that you can do in the comfort of your own home:
Administering a form of self-massage can help alleviate painful symptoms. It may not necessarily have long-lasting effects, but it can certainly help with some much-needed relief.
Most studies have shown that soft tissue treatment is most effective along the gastrocnemius and soleus muscle complex. Although it seems more intuitive to focus on the foot or ankle, massaging these calf muscles (which are both plantar flexors!) is more effective at improving pain and overall function.
That being said, if you’re looking to work these muscles, stick to performing self-massage. Many people have tried rolling an iced water bottle along their ankles and feet, but massaging the calf muscles has evidently proven to be significantly more effective.
Changing Shoes Based on Activity
Many people are recommended to simply change their shoes to help alleviate the pressure on the tissue and arches of their feet.
While this suggestion isn’t an exact science, it can help to some extent.
For starters, certain shoes with increased heel heights (like high heels or athletic shoes with a significant drop) end up adding extra pressure on the heel, so it’s important to avoid wearing shoes that have too much heel lift.
Next, make sure to rotate the kinds of shoes you wear throughout the work week. One study found that plantar fasciitis can be aggravated by wearing the same shoes every day, as this will put pressure on the same areas of your foot, ultimately causing overload.
If you’re looking for a specific kind of shoe to wear for the sake of alleviating plantar fasciitis pain, try out a pair of rocker bottom shoes. This shoe design is known to help reduce the amount of pull on the plantar fascia in combination with foot orthosis.
Conclusion
Ultimately, if you’ve been hobbling through some persistent pain along the bottom of your foot, it may be worth your time to get it checked out. Don’t let those sneaky, fluctuating symptoms push you into holding off treatment!
While plantar fasciitis pain can be stabbing and feel severe, the injury is highly probable to recover with the proper care and relief. Once you start to develop the optimal plan for alleviating the pain in your plantar fascia and allowing it to heal, you’ll be well on your way to pain-free walking and running again.
References
- Fleckenstein J, König M, Banzer W. Neural therapy of an athlete’s chronic plantar fasciitis: a case report and review of the literature [published correction appears in J Med Case Rep. 2018 Oct 1;12(1):289]. J Med Case Rep. 2018;12(1):233. Published 2018 Aug 21. doi:10.1186/s13256-018-1770-4
- Chen, H., Ho, H.-M., Ying, M., & Fu, S. N. (2013). Association Between Plantar Fascia Vascularity and Morphology and Foot Dysfunction in Individuals With Chronic Plantar Fasciitis. Journal of Orthopaedic & Sports Physical Therapy, 43(10), 727–734. doi: 10.2519/jospt.2013.4774
- Martin RL, Davenport TE, Reischl SF, et al. Heel pain-plantar fasciitis: revision 2014. J Orthop Sports Phys Ther. 2014;44:A1–33. doi: 10.2519/jospt.2014.0303.
- Wearing SC, Smeathers JE, Urry SR, Hennig EM, Hills AP. The pathomechanics of plantar fasciitis. Sports Med. 2006;36:585–611. doi: 10.2165/00007256-200636070-00004.
- Kitaoka HB, Luo ZP, Growney ES, Berglund LJ. Material properties of the plantar aponeurosis. Foot Ankle Int 1994; 15: 557-60
- Lemont, H., Ammirati, K. M., & Usen, N. (2003). Plantar Fasciitis. Journal of the American Podiatric Medical Association, 93(3), 234–237. doi: 10.7547/87507315-93-3-234
- Werner RA, Gell N, Hartigan A, Wiggerman N, Keyserling WM. Risk factors for plantar fasciitis among assembly plant workers. PM R. 2010;2:110-116. http://dx.doi.org/10.1016/j.pmrj.2009.11.012
- Salvioli, S., Guidi, M., & Marcotulli, G. (2017). The effectiveness of conservative, non-pharmacological treatment, of plantar heel pain: A systematic review with meta-analysis. The Foot, 33, 57–67. doi: 10.1016/j.foot.2017.05.004
- McKeon PO, Hertel J, Bramble D, et al. The foot core system: a new paradigm for understanding intrinsic foot muscle function. British Journal of Sports Medicine 2015;49:290.

