So you’ve gone through 6 months of rehabilitation with your local physical therapist, and they’ve given your ACL reconstructed knee the okay to go back to playing your sport.
How do you feel??
If you were to go back to full play, without limitations, how would you rate your confidence on a scale of 1-10?
If you’re feeling more nervous than excited, you’re not alone!

The vast majority of people who finish their post-op physical therapy at 6 months do not fully feel ready to go back to in-game play, and for good reason — it’s been 6-7 months (at least!) since you last played a game, and a lot has changed since then.
Plus, even though a 6-month hiatus probably felt like forever, you might also be wondering… was that enough time for your ACL to heal? You probably spent the entire six months wanting nothing more than to be back in the game, but now that you’re actually facing it, you may be questioning your preparedness.
It’s not uncommon to feel apprehensive about returning to full play after only six months of rehab. Your injury was painful and frustrating, and recovery from surgery is a long road. The last thing you want to do is re-injure your knee and go through it all again.
So, how do you know? What does science say about returning to sports after an ACL repair, and how common is a re-injury? This article will cover all of that, and more — this is a long one! Time to dive in!
Can I Still Play Sports After an ACL Surgery?
Let’s start with the best news — YES, you can definitely play a sport again after ACL surgery! Approximately 65-80% of elite athletes typically return to their previous level of competition after an ACL reconstruction. That’s a pretty great turnover from rehabilitation!
That being said, studies have shown that 12-23% of these athletes have either reduced their level of competition or stopped playing altogether by the time they reach their third year of playing post-injury. Additionally, many people don’t reach their same levels of competition as return to sport reinjury levels are around 45%.
So, while proper rehab can lead to a safe return to sport, athletes still need to consider the long-term effects of an ACL injury if they intend to play at the same competitive levels as before.
But that’s further down the road — before any of that happens, there are some factors that may put you at higher risk for reinjury of your repaired knee or injury of your contralateral knee (the other, uninjured knee).
Factors That Can Lead to ACL Reinjury
Preventing reinjury can be difficult sometimes, but knowledge is power! The next two sections are going to feel dire, but bear with us: it gets better, and it lays the foundation for why comprehensive return to sport testing is a necessity following ACL repair.
Understanding how to move correctly to help protect your joints and properly utilize your muscles will go a long way in protecting your knee. Your body’s mechanics can be super particular, especially after injury, so let’s review some of the common mechanisms of injury (MOI) for ACL tears.

About 30% of MOI are direct contact injuries, meaning that they’re unfortunately unavoidable. But that means that the remaining 70% are non-contact injuries, and these injuries are essentially caused by improper movement mechanics.
More specifically, improper mechanics are often a result of movements like decelerations or changes in direction. These movements can lead to improper knee flexion (when your knee only bends between 0-30 degrees). They can also cause tibial rotation and varus/valgus force — this means that the femur rotates inward on the tibia and the knee collapses inward. This rotation causes excessive tension on the ACL, causing it to rupture.
There are a number of other factors that contribute to neuromuscular control to prevent positions that increase the risk of injury in the knees. However, these movement patterns aren’t formally evaluated in any return to sport testing, as they are especially specific to each athlete’s sport.
There are also several general biomechanics risk factors to keep in mind, too. For example, any of the following can increase your risk of reinjury (or injury of the other knee):
- decreased knee and hip flexion
- increased knee valgus (internal rotation and adduction)
- increased hip internal rotation
- increased quadricep activity (overuse of quadriceps)
- decreased gluteus maximus activity (underuse of gluteals)
Even after rehabilitation, an ACL injury can still create vulnerabilities for an athlete, so make sure your joints and muscles are moving properly — they’re imperative to executing sport-specific movements safely!
Occurrence of ACL Rupture After Return to Play
Of course, considering your biomechanics won’t guarantee reinjury prevention — but nothing will. Technically, there’s always a chance of rupture when returning to sport. While that may not be what you want to hear, the statement is true whether you’re post op or have never been injured before.
So, is there any method to the madness?
There are some factors that have been correlated with a higher risk of reinjury. For example, rupture can occur based on age alone — when an athlete is under 20 years of age, they are 3-6 times more likely to experience ruptures after return to play. Some reports state that the reinjury rate for children and young adolescents is as high as 30%.
That, and you’re generally at higher risk for ACL injury within the first 2 years of return to sport — you’re 6 times more likely to experience an ACL injury of either ACL during that time frame.
But that’s strange, isn’t it? Typically, you will have gone through the usual ACL return to sport testing, yet there are still such high rates of reinjury within the first 2 years of return to sport.
This then begs the question… is it right to be pushing for an accelerated return to sport program?
It’s fair to wonder, especially if you’re the one that’s prone to reinjury. Plus, there’s research that actually backs up that exact concern.
In one study, 49 athletes were tested between 5-11 months after ACL reconstruction — only 14.3% passed the return to sport criterion within 6 months. And while 6 months sounds pretty great to an eager-to-return athlete, the success rate of that short a time period makes it seem much less ideal for effective rehabilitation.
Additionally, 100% of the athletes that returned to sport less than 5 months after surgery suffered reinjury or contralateral ACL injury just within their first 2 months of return to sport. From there, the researchers (unsurprisingly) determined that the reinjury rate had reduced by 51% for every month that return to sport had been delayed (testing up to 9 months after surgery).
So, knowing how the timeline for return to sport can drastically impact an athlete’s chances of reinjury, it’s important to question the current structure of return to sport protocol. Why do people continue using accelerated programs if they’re proven to be ineffective? What do these protocols really consist of, and why aren’t they better at lowering risk of reinjury?
Typical Return to Play Protocol for Post-Op ACL
Currently, the return to play protocol consists of four types of assessments:
- The Knee Outcome Survey
- The Noyes Hop Test
- The Landing Error Score
- The Limb Symmetry Index
Each assessment is intended to measure its own aspect of performance — ideally, that means that physical therapists can determine what needs to be worked on for proper rehabilitation, right?
(You know where this is going…)
We hate to be the bearer of bad news, but most of these assessments lack a proper evaluation of specific movements and abilities needed for return to sport. Sure, these tests may measure an athlete’s general capabilities and indicate some improvement throughout rehabilitation, but they neglect to factor in necessary aspects for sport-specific movements.
The Knee Outcome Survey Activities of Daily Living Scale
First up is a self-evaluation questionnaire called the Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL). Basically, the KOS-ADL records a general idea of how different pain symptoms affect your level of activity on a day-to-day basis.
The harder a task is due to your knee pain, the lower your score is. Once you complete the form, you add up your points, and your total will then allow you to determine a percentage of disability with everyday activities.
The higher your percentage, the less disability you experience in daily activity; conversely, the lower your percentage, the more disability you experience in the knee. This questionnaire also has a sports activity subscale that functions in the same way.
The data collected through a self-reported questionnaire can be skewed from person to person — people perceive pain and difficulty differently, and individuals may be tempted to misrepresent their experience in order to be cleared sooner. Self-reported information will always be part of rehabilitation, but it lacks concrete, data-backed information on the progression and capabilities of the knee.
The Noyes Hop Tests
In terms of more specific testing, one of the standard assessments is the Noyes hop tests, which comprises 3-4 types of hop tests (as pictured). Tests A (single-leg hop), B (triple hop), and C (crossover hop) are used to measure distance. Test D is a 6-minute hop used to measure time.
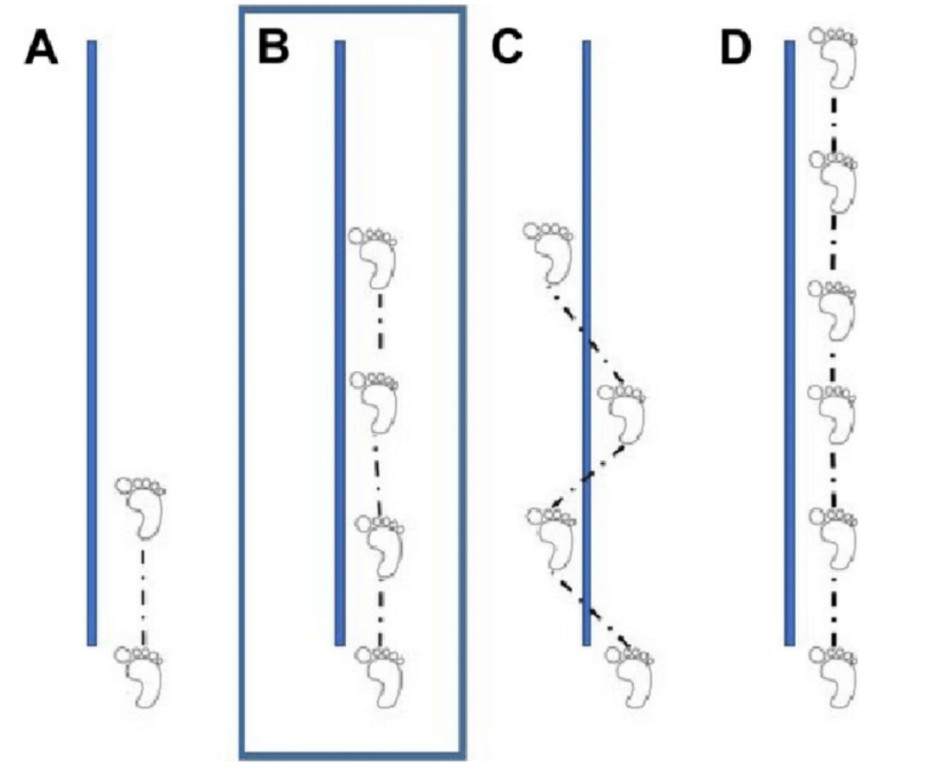
In order to pass each test, an athlete must meet 90% or more symmetry to the performance of their uninjured leg.
These hop tests are correlated with self-report questionnaires about knee function, but they aren’t specifically linked to return to sport statistics. Plus, none of them actually replicate a majority of the movements that athletes will perform during a full speed play of their sport.
In the end, they neglect to evaluate the quality of sport-specific movements, which is a key factor in initial injury and reinjury. While they can certainly be helpful to assess general athletic ability, they ultimately can’t serve as a direct indicator of whether or not an athlete can return to play, so it defeats the purpose of including it in return to sport protocol.
The Landing Error Scoring System (LESS)
In addition to those individual hop assessments, some test batteries will also include jump-landing tasks scored by the Landing Error Scoring System (LESS).
The acronym for this test is true to the goal — in order to pass, you need to score five or less! A higher score represents a greater number of movement errors.
This testing looks at the quality of your functional movement by assessing potential errors in both jumping and landing movements. It looks at your trunk, knee, and hip position for both initial landing contact and overall shock absorption.
Generally, this method results in similar or consistent scores across multiple tests and clinicians, so it has a relatively high reliability. Unfortunately, the jump maneuvers of this test aren’t a single-leg task like most sports movements, so the test still lacks an accurate replication of sport-specific movements (which would be pretty important to know when returning to sport).
It’s on the right track, but still hasn’t reached the destination just yet!
The Limb Symmetry Index (LSI)
Lastly, there’s the isokinetic quadricep test, otherwise known as the Limb Symmetry Index. This index measures the strength and max contraction of the quadricep on the injured side. That data is then compared to the data of the uninjured side.
In order for an athlete to pass this assessment, the quadricep on the injured side must have 90% or more of the strength exhibited on the uninjured side.
However, there’s a common issue with this test — after 6 months of rehabilitation, your lack of sports activity will have weakened your contralateral (uninjured) leg. This means that the test is comparing your injured leg to a lower level of strength, so even if it passes with 90% or more strength, your legs still wouldn’t be as strong as they were preinjury. And that definitely isn’t ideal if you’re trying to get back to playing at your usual intensity.
But on the bright side, there’s an alternative assessment! Instead of the LSI, it’d be better to use the EPIC levels system — it compares the strength of the ACLR leg (post-rehab) to the strength of the contralateral leg BEFORE the injury, so it’s much more accurate for the purposes of returning to sport.
For example, in one study, 57.1% of the patients were able to pass LSI and hop testing at just 6 months. But, with the EPIC levels system, only 28.6% of patients were able to meet 90% at 6 months.
While these assessments can provide solid data, they still basically only assess whether or not your muscle strength is equal in both legs. Neither of these tests directly evaluate the ability of the injured quadricep to be used during full speed activities, nor do they assess its ability to control the knee and prevent potential reinjury.
And on top of that, there’s more to consider…
One study found that the average maximum isometric force from quadriceps (MVIC) was about 97% of the strength of the pre-injury, contralateral leg at just 6 months. That looks pretty good, right? Well, that statistic alone is a great result, but it really only measures one specific ability.
In addition to quadricep strength, athletes need to match previous levels of rate of force development (RFD), which is how quickly their muscles can produce force. This RFD ability is way more significant and relevant for sports — it allows athletes to make quick movements like cutting, jumping, or sprinting. Unfortunately, current return to sport testing doesn’t even begin to evaluate RFD.
What is Proper Return to Sport Testing?
Whew, that was a lot to take in! Let’s pause for a second.
All of that information isn’t meant to scare you out of playing again. It just means that you’re totally justified to feel unprepared for return to sport — if you only go through those unspecific, accelerated assessments, you actually AREN’T prepared to!
But good news — testing is catching up to the science! There is current technology available that allows for accurate AND comprehensive return to sport testing; it’s what we use at Competitive EDGE. Our goal is to make sure that we assess the sport-specific movements that each individual athlete will utilize during their full intensity game play, ensuring that they have sound mechanics (even at game speed) and can safely return to play. Unfortunately, it hasn’t become the industry standard for testing yet. Big changes take time.
In the meantime, let’s look at what true athletic return to sport testing encompasses, and how it’s implemented.
Specialized Technology for Accurate Data Collection
Step one of reliable, data-driven return to sport analysis is getting the most accurate information possible.
No matter how sharp a physical therapist’s eyes may be, we inevitably can’t catch every intricacy of an athlete’s mechanics just by watching. So, our goal is to take the subjectivity and bias out of the evaluation processes with the use of 3D motion capture and an inertial measurement units (IMU) system.
Many specialists will often use video to draw angles that represent dorsiflexion, knee flexion, and hip flexion, but these drawings are all ball-park estimates at best. An IMU system, on the other hand, creates a visualization of an athlete’s skeletal structure and collects precise angle measurements of each joint in a 3D space to within 1° of motion! Couple that with a built-in force plate that helps us detect the direction and magnitude of forces and high-speed cameras, and you have the full picture of an athlete’s mechanics — free of bias.
Super cool, right?

But obviously, all this specialized technology isn’t just here to collect data. We use the information collected to analyze an athlete’s proficiency and biomechanic soundness in a variety of sport-specific scenarios. Because we’re able to gather such specific information about individual athletes’ mechanics, we can see specific areas that need to improve to pass the assessment. It also allows us to plan physical therapy sessions focused on areas that need improvement in order to safely return to play.
Sport-Specific Test Parameters
Chris Powers utilizes a specific protocol that scores and assesses multiple categories, including hip stability, shock loading, trunk stability, hip strategy, and pelvis stability. All of these categories are essential for ensuring proper movement mechanics and promoting lower extremity alignment to reduce the risk of injury. And, of course, for checking whether or not an athlete can safely return to their sport at the top of their game!
This comprehensive return to sport assessment involves 6 sport-specific movement tests:
- Step Down/Single Leg Squat off an 8” Step — This stepping movement assesses single leg stability and mechanics.
- Drop Jump off an 18″ PlyoBox — This jump-landing movement measures shock loading and evaluates lower extremity hip strategy.
- Lateral Shuffle with Change of Direction — This sideways movement assesses frontal plane movement.
- Sprint to Deceleration to Backpedal — This forwards and backwards movement assesses sagittal plane movement.
- Triple Hop — This vertical movement tests dynamic plyometric stability.
- 90 Degree Cut — This is a sport-specific, 3D movement with cutting, and it’s the primary method of injury for most athletes. A formal assessment of this movement ensures an athlete’s safety in return to play.
Depending on the athlete’s sport, it’s also best to include testing for additional movements that replicate specific sports play for further assessment.
Additionally, there are a variety of tests performed with the force plate:
- Reactive Strength Index — This index pinpoints how well an athlete is generating power by assessing the RFD (rate of force development) of the lower extremity.
- Time to Stabilization — This test focuses on the lower extremity through single-leg jumping to assess balance and neuromuscular control; the results are then compared to the uninjured side.
- Squat Symmetry — Often after injuries such as ACL, athletes have a tendency to rely on their uninjured side, which can be a huge injury risk and often a primary reason for the high occurrence of contralateral leg ACL tears following the first ACL tear. This test helps determine the current state of the uninjured leg.
- Jump Symmetry — This jump test assesses how much force each leg generates, how well they absorb forces, and if they absorb the forces equally.
- Y-Balance Testing — This test evaluates 3D single leg balance, mobility, and stability.
- Triple Hop — In addition to being a sport-specific movement, this test also assesses an athlete’s overall distance for force production and leg symmetry.
These comprehensive tests not only help to assess the quality of each specific movement, but it also allows the physical therapist to identify which aspect of the movement needs to be improved upon.
And, just as importantly, there is a full physical therapy evaluation for the athlete in addition to the testing. This includes an assessment of range of motion, strength, and neuromuscular control.
Using all of this information, each athlete is scored a number of points out of a total of 50 based on their sport movement assessment with our IMUs and the other functional tests:
- If they score below 35 points, they are placed in the High/Substantial Risk Category. A majority of athletes land in this category at the 6-month Sport Test, especially those with ACL injuries!
- If they score between 35-44 points, they are in the Moderate Risk Category.
- If they score between 45-50, they are within the Low Risk Category.
All together, these tests and scores will break down each individual movement to help determine what improvements are needed to result in the best, safest, and most powerful movement. Not only does this provide the athlete with knowledge about their individual movements, but it also helps the physical therapist direct their personalized plan of care to ensure the most effective recovery. With all this specific data, the therapists can dedicate their work to safely and properly rehabilitating an athlete!
Return to Play Progressions
Now that you know how thorough return to sport testing should be, you’re probably starting to wonder how long all of that must take, right?
Below is the general timeline and benchmarks for ACL protocol:
- After 6 months, we will perform RTS initial testing.
- At 6-7 months, they will work on increasing speed and motor control training — this will include double- to single-leg plyometrics, multi-direction agility drills (at 50-75% speed), and sports-related practices (at 50-75% speed).
- At 8 months, they will undergo cardiovascular training and continue with an increased speed of sport-related play.
- At 9-12 months, they will focus on several tasks — game speed practice (at 100% speed); sprinting to decelerations, shuffling, cutting, and jumping; and finally RTS testing for clearing for sport.

By collecting objective data, physical therapists can track an athlete’s progress and provide concrete numbers to support when returning to sport is most feasible.
We know that a year sounds like a long time, but avoiding reinjury is well worth the extra time. Remember that an accelerated (and inaccurate) ACL protocol pushes athletes to return to sport far earlier than they should, which only increases the probability of reinjury.
With all the unfun experiences that come with an ACL injury, make sure you do what you can to prevent reinjury! Allow your body some more time to recuperate — it’ll thank you in the long run!
In Conclusion
Congratulations, you made it through this beast of an article!
Let’s check in — how’re you feeling about returning to sport now?
Now you know the grim truth behind current return to sport protocol, BUT you also know that there are concrete, data-based methods that can help you avoid those pitfalls! If you’re determined to return to sport, find comfort in knowing that you can 100% get there.
Just remember that proper return to play takes time! To avoid rushing and reinjury as much as possible, the primary goal is to ensure that every athlete has the proper time and practice to be fully prepared to return to the highest level of play.
So fear not, warrior — with the proper thoroughness and procedure, you’ll be well on your way to getting back to your favorite sport!

